From Incident to Resolution,
APS Is Your Solutions Provider
APS is a comprehensive, end-to-end business process automation firm focused on workers’ compensation and auto casualty claims.
We were founded with the simple, yet powerful mission of reducing the cost of risk for our clients.

Automate the Entire Medical Bill Cycle
… with a fully integrated paper-to-electronic and eBill solution
Combining our end-to-end solutions and our innovative technology creates a powerful suite of tools that will enhance your workflow and save you money!
With our Clearinghouse solution, Payments services, Digital Mailroom (centralized document intake), Print and Mail solution, and AP Capture platform, along with our document services, Bill Review and Negotiation, and our claims processing product, APS truly takes the claims management process from inception to resolution.
What You Can Achieve With Our Expert Solutions
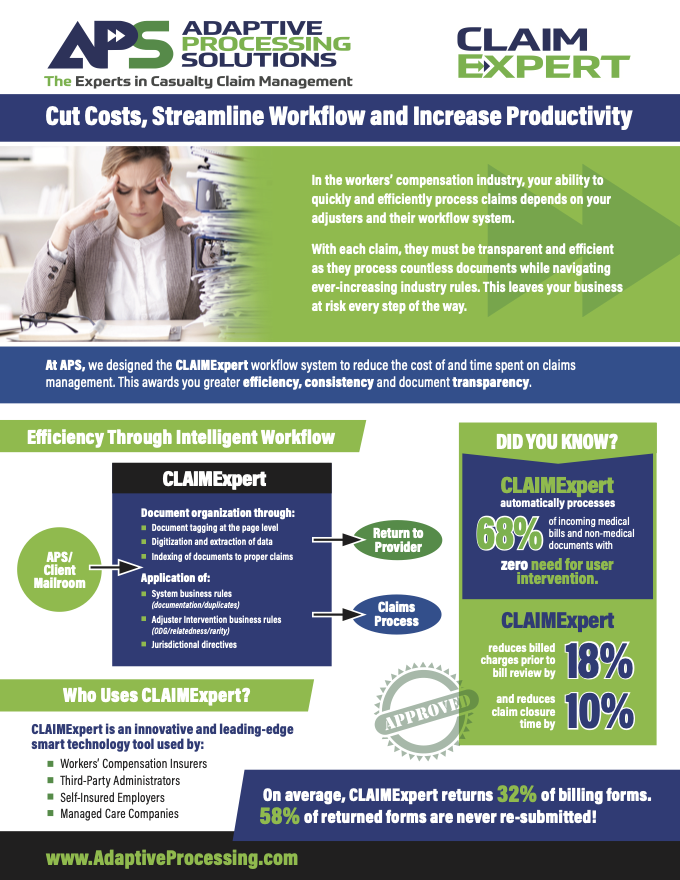
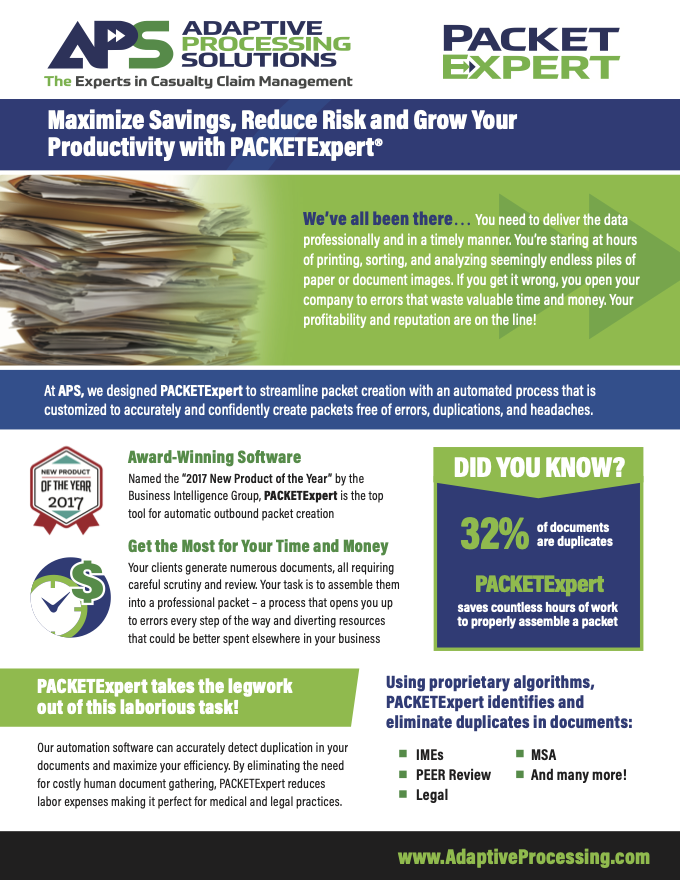
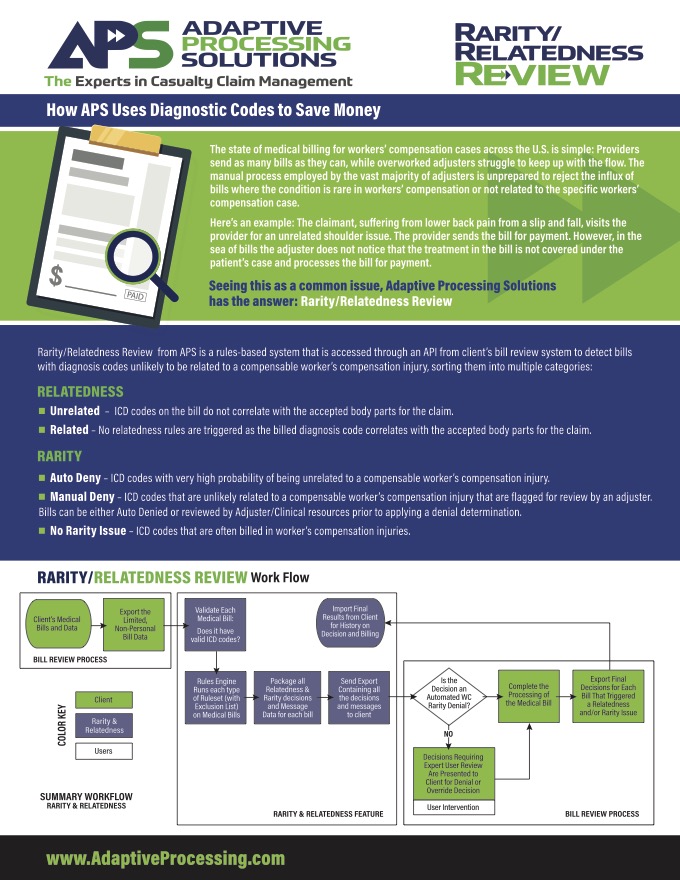
Our claims processing solutions are remarkably flexible and effective. Each of our expert, rules-based software solutions are designed to create meaningful changes to your workflow productivity to help you stay relevant and adaptive in today’s everchanging marketplace.
Reduce Medical Spend by 21%
Maximize Adjuster Effectiveness
Close Claims 10% Faster

Do you have problems with…
Medical loss and leakage?
Inefficiencies in your claims process?
Lack of transparency into vendor performance?
Overworked adjusters?
Product Spotlights
Reducing Your Cost of Risk
Solutions for Insurers
Today’s insurers are facing a tough environment. We’ve got the solutions that will help you succeed no matter what problems you’re facing.

Solutions for Self-Administered
Our solutions help Self-Insured and Self-Administered organizations overcome obstacles and achieve their goals.

Solutions for TPAs
At APS, we understand the challenges facing Third-Party Administrators in today’s business environment. We offer a variety of tools and solutions to improve your operations and ensure success.

Solutions for Managed Care
APS works with many Managed Care Companies and we are attuned to the unique challenges and goals that you may have.